Cold plasma successful against brain cancer cells
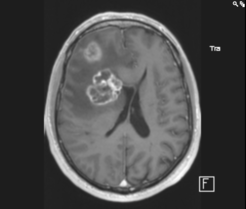
If someone is diagnosed with the type of brain tumour called glioblastoma, the prospects are dire: median survival is just a bit over one year, and less than 16 % of the patients survive more than three years. It is still unknown how this cancer is triggered – only a few rare genetic factors have been identified so far – and treatment remains largely palliative, i.e. trying to alleviate the symptoms and prolonging the life of the patient. The standard therapy proceeds in three steps: Guided by an MRT scan, the tumour is removed surgically, followed by radiation and chemo therapy. But even if the treatment is successful initially, there is a high likelihood of relapse.
A recently developed new kind of treatment could offer some hope. Cold atmospheric plasma, or CAP for short, has already proven to successfully inactivate bacteria, fungi, viruses and spores, while healthy tissue remains largely unaffected. Healthcare applications such as the sterilization of surgical instruments, skin and wound disinfection paved its way into medical care. Recently also CAP sources were developed which show anti-cancer properties.

"For many patients the regular treatment is just not effective, because the brain tumours contain sub-populations for which chemo therapy does not work,” says Julia Zimmermann, who manages the Plasma Healthcare group at MPE. “So we were particularly interested to see if the CAP would be effective against these resistant tumour cells – and indeed it worked!”
For the study, the researchers used Glioblastoma cells and grew them in cell culture dishes, where they could be subjected to various combinations of treatments. For both normal and resistant tumour cell lines, the growth of the cells was more inhibited after the plasma treatment compared to the chemo therapy alone. The largest effect could be obtained for a short application time of 120 seconds; such an additional step could be easily incorporated into the clinical treatment if an appropriate plasma device can be developed.

The researchers also found that CAP stops the cell cycle and that the individual cells lose their ability to clone themselves. A combined therapy of both - CAP treatment and chemo therapy – showed the most promising results, where the amount of chemotherapeutic needed to achieve the same result as with chemo therapy alone is strongly reduced. So far, no resistance towards CAP treatment was observed. The study also showed that even those cell lines that originally were resistant against the chemo therapy drug became sensitive again after the pre-application of CAP.
“In particular, also resistant cell populations could be treated effectively with CAP, which means that there is now hope to find a therapy for the patients with a poor prognosis, i.e. those with resistant cells in the tumour,” explains Julia Köritzer, lead author of the study. Such a treatment option for resistant cells is urgently needed, because about 40 % of the patients do not profit from chemo therapy. She adds: “It is a first step, now we have to further investigate the effects gained in the cell culture and integrate them for the application.”
Though, even if there is still a long way ahead before CAP can actually be used in the hospital, it offers a promising new possibility. Eventually it could be applied after surgery to treat the tissue around the extracted tumour, where some cancerous cells might have been left behind, preventing the cancer from reappearing. Devices similar to an endoscope are currently under development.


